Movements of GIT involves:
- Oral cavity
- Esophagus
- Peristalsis
- Mixing movement
- Stomach
- Small intestine
- Large intestine
- Motility of GIT
- Propulsion movement
Movements of the gastrointestinal tract
As part of its digestion and absorption, the gastrointestinal tract (GIT) chews food and mixes it with saliva (mastication), swallows, and moves food around.
Through the esophagus and stomach, where digestion begins, foods pass through the small intestine (where they are digested and absorbed). Upon passing through the small intestine, food travels to the large intestine, where it is digested and excreted into the rectum. Food must be propelled and moved (motility) from one end to the other of the tract through these parts. In the gastrointestinal tract, the term "gut motility" is associated with muscle contractions and stretching. These contractions are synchronized and are termed peristalsis. The digestive tract is responsible for allowing food to move along while at the same time absorbing nutrients. By measuring the contraction of each region of the gut, we can identify the normal pattern of contractions. The types of gut contractions vary according to the type of food eaten and the region. in some contractions, the food moved forward and along with it, it mixes and grinds well during the process. there are four types of major regions in the GI tract that include - the esophagus, the stomach, the small intestine, and the large intestine. Special muscles called sphincters separate them from one another and control the movement of ingested materials between them. As each part of the GI tract performs a different function of indigestion, it also has a distinctive form of motility and sensation.
Duodenum - First, the chyme passes through the duodenum, an area where digestive secretions aid digestion. Bicarbonate, enzymes, and bile salts are all included in the secretions. A, D, E, and K vitamins (fat-soluble vitamins) are digested by the liver's bile salts. The pancreas produces enzymes that help with this process. Carbohydrates and fats are digested by pancreatic enzymes. Acid from the stomach is neutralized by bicarbonate from the pancreas.
Jejunum - Further transit of the chyme takes place in the jejunum, which is the second part of the small intestine. in the first half of the jejunum, there is the majority of the number of nutrients that get absorbed that also includes carbohydrates, proteins, minerals as well as vitamins.
Ileum - The large intestine is connected to the colon. The small intestine ends with the ileum. In addition to absorbing water, bile salts, and vitamin B12, the ileum also performs several other functions. Located in the first portion of the colon, between the ileum and the cecum, the ileocecal valve is a one-way valve. As a result of this valve, contents are controlled from passing into the colon, and nutrients and electrolytes (essential minerals) can contact the small intestine for longer periods. As well, it minimizes bacterial movement from the large intestine into the small intestine by preventing back-flow (reflux) from the colon into the ileum. Upon arriving from the ileum, contents from the large intestine are stored here. Unlike the small intestine, the cecum forms in a pouch-like shape. Water and electrolytes, especially sodium and potassium, are absorbed by the large intestine, and luminal contents are converted into firmer stools by the large intestine. It spends about one and a half liters (about one and a half quarts) of fluid a day and if necessary, can absorb up to five liters or quarts, depending on the needs. In addition to digesting dietary fiber (fermenting it), the colon creates short-chain fatty acids that are absorbed and add nutrition to the body. The colon's pattern of contraction is less well understood than that of the small intestine. However, eating a meal can stimulate colonic contractions, and the larger the meal, the greater the response. Stretching the rectum using a stool relaxes the anus and surrounding muscles. As a result, the contents of the rectum can be released voluntarily.


Celiac disease - A person with celiac disease has hypersensitivity to gluten in the small intestine due to an autoimmune disorder. Gluten contributes to the body's immune system attacking the small intestine, which damages the villi which facilitates nutrition absorption. Children with celiac disease can experience bloating, constipation, rash, weight loss, and a decreased growth rate. Celiac disease is currently treated only by following a gluten-free diet for the rest of one's life.
Constipation - Constipation means having difficulty passing stools (feces) or passing them infrequently. It varies from person to person how long passes between bowel movements before constipation occurs for those who do not have daily bowel movements. Constipation causes small, hard, dry, and difficult-to-pass stools. Additionally, some people may experience bloating or distention in their stomachs as well as pain during their bowel movements. Constipation is often associated with hemorrhoids. Your constipation should be diagnosed as soon as possible. Dehydration, lack of fiber in your diet, pregnancy, inactivity, and medications (such as opioids, iron supplements, or antidepressants) are some factors to consider. It is possible to relieve constipation with laxatives and to prevent it from returning with lifestyle changes.
Crohn's disease - Chronic bowel disease, Crohn's disease causes inflammatory patches in the GI tract anywhere from the mouth to anus, although it is most commonly found on the junction where the small intestine meets the large intestine. According to experts, the exact cause of the disease is unknown; however, it is more common in "Westernized" countries, runs in families, and can be aggravated by diet and stress. There are several symptoms associated with this condition, including diarrhea lasting several weeks, abdominal pain, and weight loss. Around 50% of those with Crohn's disease, notice blood in their stools or mucus in their stools, and some may feel as if they are not able to evacuate completely. Among the various kinds of drugs available for treating arthritis are aminosalicylates, steroids, immunomodulators, and biologics. In addition, surgery is an option.
Diarrhea - Diarrhoea is marked by frequent urgency to go to the toilet as well as loose, watery stools (feces). Sometimes nausea or vomiting can also occur, as well as abdominal pain or cramps. Noroviruses, which are a common cause of diarrhea outbreaks on cruise ships, are a common cause of diarrhea caused by viruses. Salmonella, campylobacter, or Escherichia coli are common causes, as are giardia; various medical conditions (including celiac disease); food intolerances, and certain medications. Loperamide and diphenoxylate slow down bowel movements, while electrolyte solutions treat dehydration associated with diarrhea, which typically occurs after excessive diarrhea. There may also be a need for other medicines, such as antibiotics.
Gastroesophageal reflux disease - Heartburn and acid reflux are also known as GERD. The lower esophageal sphincter, which normally closes tightly to prevent food from flowing back up the esophagus, becomes weakened and remains partially open. This allows partially digested food and stomach acid to leak back up and cause irritation. Regurgitation, heartburn, chest pain, and nausea are the primary symptoms associated with GERD. Antacids, H2 blockers, and proton pump inhibitors are most commonly used to treat GERD.
Through the esophagus and stomach, where digestion begins, foods pass through the small intestine (where they are digested and absorbed). Upon passing through the small intestine, food travels to the large intestine, where it is digested and excreted into the rectum. Food must be propelled and moved (motility) from one end to the other of the tract through these parts. In the gastrointestinal tract, the term "gut motility" is associated with muscle contractions and stretching. These contractions are synchronized and are termed peristalsis. The digestive tract is responsible for allowing food to move along while at the same time absorbing nutrients. By measuring the contraction of each region of the gut, we can identify the normal pattern of contractions. The types of gut contractions vary according to the type of food eaten and the region. in some contractions, the food moved forward and along with it, it mixes and grinds well during the process. there are four types of major regions in the GI tract that include - the esophagus, the stomach, the small intestine, and the large intestine. Special muscles called sphincters separate them from one another and control the movement of ingested materials between them. As each part of the GI tract performs a different function of indigestion, it also has a distinctive form of motility and sensation.
Oral cavity
Chewing, mixing saliva with food, and swallowing begins the digestion process. In the oral cavity, food is selected, ground, and partially digested. Mastication is a term used to describe the grinding of food. The enzyme salivary amylase, which aids in the semi-digestive process of starch, lubricates and starts chemical digestion. The food pieces are then gathered together into spherical masses called boluses.Pharynx and esophagus
In addition to swallowing, food enters the stomach via the esophagus after passing through the mouth. Eating is not digested by the esophagus; saliva continues digestion. An alimentary canal wall's smooth muscles contract and relax during peristalsis. Peristalsis occurs during the passage of food from the mouth to the rectum.Stomach
Food eaten at each meal can be temporarily stored in the stomach. there are many powerful contractions taking place in the lower part of the stomach where the solid particles of the food are broken down gradually. Right after the muscular activity where the small food particles are made-up, nutrient absorption begins right after that inside the small intestine. At many different rates, different types of food materials pass through the stomach; just like fat that takes a much longer time to digest than the other types of food. Unlike food, beverages are handled differently by the stomach, going directly into the small bowel without needing to be broken down into smaller parts. About two hours after a standard-sized meal, most of it has left the stomach. It is while the food is being digested (parsed) in the stomach that the digestive juices such as hydrochloric acid and digestive enzymes like pepsinogen are released. Pepsinogen is converted into active pepsin by the release of HCL. Chyme is the name given to the mixture.Small intestine
After passing through the stomach, chyme moves into the small bowel/intestine in a controlled manner. Small intestinal muscle contractions occur irregularly, and the strength and type of contractions vary. The type of contractions generated by food depends on the nutrients present. A medium-sized meal causes contractions that last several hours, mixing and moving food through the digestive tract. Typically, these contractions last until the majority of the meal residues have made their way into the large intestine. It takes different foods different amounts of time to travel along the small intestine movement of fat-rich foods is slower than the movement of fiber-rich foods. The contractions of the stomach change once most of the food has been absorbed by the small intestine. During fasting, and particularly at night, the intestines are subject to powerful contractions every 90 minutes. In this way, these bursts act as a "housekeeper" in the intestine, removing all food and secretions remaining from the upper intestine. Adults have an average length of about 7 meters/22 feet for their small bowel. in total, there are approximately three segments in the small intestine such as,- The duodenum
- The jejunum
- The ileum
Duodenum - First, the chyme passes through the duodenum, an area where digestive secretions aid digestion. Bicarbonate, enzymes, and bile salts are all included in the secretions. A, D, E, and K vitamins (fat-soluble vitamins) are digested by the liver's bile salts. The pancreas produces enzymes that help with this process. Carbohydrates and fats are digested by pancreatic enzymes. Acid from the stomach is neutralized by bicarbonate from the pancreas.
Jejunum - Further transit of the chyme takes place in the jejunum, which is the second part of the small intestine. in the first half of the jejunum, there is the majority of the number of nutrients that get absorbed that also includes carbohydrates, proteins, minerals as well as vitamins.
Ileum - The large intestine is connected to the colon. The small intestine ends with the ileum. In addition to absorbing water, bile salts, and vitamin B12, the ileum also performs several other functions. Located in the first portion of the colon, between the ileum and the cecum, the ileocecal valve is a one-way valve. As a result of this valve, contents are controlled from passing into the colon, and nutrients and electrolytes (essential minerals) can contact the small intestine for longer periods. As well, it minimizes bacterial movement from the large intestine into the small intestine by preventing back-flow (reflux) from the colon into the ileum. Upon arriving from the ileum, contents from the large intestine are stored here. Unlike the small intestine, the cecum forms in a pouch-like shape. Water and electrolytes, especially sodium and potassium, are absorbed by the large intestine, and luminal contents are converted into firmer stools by the large intestine. It spends about one and a half liters (about one and a half quarts) of fluid a day and if necessary, can absorb up to five liters or quarts, depending on the needs. In addition to digesting dietary fiber (fermenting it), the colon creates short-chain fatty acids that are absorbed and add nutrition to the body. The colon's pattern of contraction is less well understood than that of the small intestine. However, eating a meal can stimulate colonic contractions, and the larger the meal, the greater the response. Stretching the rectum using a stool relaxes the anus and surrounding muscles. As a result, the contents of the rectum can be released voluntarily.
Gastrointestinal motility
In the human body, motility is defined as the involuntary movement of certain tubular organs. For food to be digested efficiently, active enzymes must be present along with the shift and mixing of chyme as it passes through the digestive tract. During the GIT movement, there are two kinds:- Propulsion movements
- Mixing movements
Propulsion movements
During digestion, propulsion movements allow chyme to move through the digestive tract. The rate of absorption and digestion will be proportional to it. Peristalsis is the basic motion of propulsion. An aboral contractile ring is formed when the circular muscle at a certain place contracts. The contractile ring is then moved aboralward. A subsequent movement of the chyme occurs. Peristalsis is often triggered by intestinal distension - and the formation of the contractile ring as a result. Distension of the gastrointestinal tract is often the catalyst for the formation of the contractile ring, and hence for the beginning of peristalsis. Distention is caused by a large amount of chyme and is a result of chyme stimulating the enteric nervous system. The circular muscle segment is contracted by this force, which is located a few inches orally from the point where the tube expands maximally. A strong parasympathetic activation or chemical stimulus can also trigger peristalsis. It is also triggered automatically periodically. Moreover, receptive relaxation of the distended segment occurs abnormally in addition to oral contraction. It is easier for the chyme to move when the tube is relaxed since the moving chyme is less resistant. Auerbach's plexus (or myenteric plexus) is responsible for controlling the whole process, which is referred to as the peristaltic reflex. Experiments have shown that propulsion movements can also occur in the oral direction, but they vanish within a few millimeters. Hence, peristaltic movements are unidirectional, though the physiological mechanisms by which this occurs are not fully understood.Mixing movements
During mixing, chyme is constantly mixed to ensure that it is continually exposed to enzymes and comes into contact with the intestinal wall to become absorbed. Digestion consists of different movements that occur in a variety of forms.Digestion and absorption of nutrients
Ingested food is broken down into absorbable molecules through digestion. The absorption of nutrients, water, and electrolytes occur when the mucosa of the small intestine moves to the cells, then into the bloodstream.Carbohydrates
Digestion
Gastric digestion of carbohydrates includes the absorption of glucose, galactose, and fructose. Three types of sugars are absorbed by the small intestine: glucose, galactose, and fructose. It is in the mouth that starch is digested, where salivary amylase is involved. Small intestines are responsible for most carbohydrates digestion. A brush border enzyme converts all the disaccharides produced (maltose, maltotriose, and α-dextrin) into glucose. Amylase does not break down naturally occurring disaccharides in food. The brush border enzymes (lactase, sucrase, trehalase) hydrolyze these compounds into glucose, galactose, and fructose.Absorption
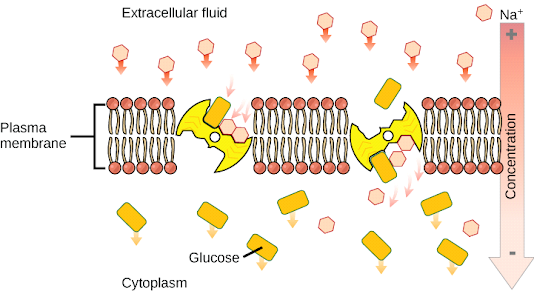
By using primary active transport (along with Na+) to transport glucose across apical membranes, the sodium-glucose cotransporter (SGLT1) transports glucose and galactose. Through the basolateral membrane, glucose and galactose leave the cell and enter the bloodstream. Sugar is transported from the cell to the blood by GLUT2 receptors through facilitated diffusion via GLUT5.Proteins
Digestion
A stomach enzyme called pepsin begins the digestion of protein by breaking it into amino acids and oligopeptides. As part of the digestive process, the small intestine uses brush border and pancreatic enzymes. Separating oligopeptides is achieved by splitting them into amino acids, dipeptides, and tripeptides.Absorption
In a similar manner to how monosaccharides are absorbed, amino acids are absorbed through a sodium cotransporter. Facilitated diffusion is then used to transport them across the membrane. Separate H+ cotransporters are involved in dipeptide and tripeptide absorption; once inside the cell, they are hydrolyzed to amino acids.Lipids
Digestion
Because lipids are hydrophobic, they are poorly soluble in digestion's aqueous environment. Lipids are digested by lingual and gastric lipases, but only about 10% of the total lipids are digested. The small intestine digests the remaining lipids. In this case, bile emulsifies a fat globule into micelles, which have a vastly increased surface area, and thus aids in digestion. Micelles are reduced to fatty acids, monoglycerides, cholesterol, and lysolecithin during lipolysis by various enzymes such as pancreatic lipase, phospholipase A2, and cholesterol ester hydrolase.Absorption
At the apical membrane, digestive products are released and diffuse into the enterocytes. Inside the cell, the lipids, triglycerides, cholesterol, and phospholipids are re-esterified to form their original forms. A chylomicron is formed by packaging lipids inside apoproteins. Chylomicrons are too large to enter the circulatory system, so they are transported via lacteals to the lymphatic system.Water absorption
Adults usually consume approximately 1-2 liters of water each day, but their small intestines absorb 9 to 10 liters of fluid per day, of which 8 to 9 liters are due to GI secretions. It is mainly the small intestine that absorbs water and electrolytes, and some water is also absorbed by the colon. Solutes like Na+ and Cl-, which absorb water, contribute to water absorption. Cotransport of Na+ ions with glucose and amino acids facilitates Na+ ion movement into enterocytes from the intestine, as well as Na+/H exchange, which facilitates Na+ ion movement into the enterocytes. Na+ is rapidly pumped out of the enterocyte by the sodium pumps, allowing water to follow through osmosis via transcellular or paracellular pathways (between the tight junctions of the enterocytes). This allows for the diffusion of both water and Na+ ions into capillaries.Disorders of GIT
Disorders of the gastrointestinal tract are commonly referred to as gastrointestinal disorders. This is the term used for the long, continuous passage that runs from our mouth to our anus, called the gastrointestinal tract (or GI tract). We have a mouth, small intestine, stomach, and esophagus, large intestine, and anus that are all part of our GI tract. This is the term used for the long, continuous passage that runs from our mouth to our anus, called the gastrointestinal tract (or GI tract). Nerves and hormones play a critical role in the function of the digestive system, while bacteria that live within the GI tract (gut flora or microbiome) play an equally critical role in digestion, immunity, and our general well-being. A membrane called the peritoneum holds the digestive system organs in place. Some many conditions or diseases can affect digestion or our overall health that can affect the gastrointestinal tract. It may take further testing to determine the diagnosis of certain conditions whose symptoms are similar. Digestive disorders include the following:Celiac disease - A person with celiac disease has hypersensitivity to gluten in the small intestine due to an autoimmune disorder. Gluten contributes to the body's immune system attacking the small intestine, which damages the villi which facilitates nutrition absorption. Children with celiac disease can experience bloating, constipation, rash, weight loss, and a decreased growth rate. Celiac disease is currently treated only by following a gluten-free diet for the rest of one's life.
Constipation - Constipation means having difficulty passing stools (feces) or passing them infrequently. It varies from person to person how long passes between bowel movements before constipation occurs for those who do not have daily bowel movements. Constipation causes small, hard, dry, and difficult-to-pass stools. Additionally, some people may experience bloating or distention in their stomachs as well as pain during their bowel movements. Constipation is often associated with hemorrhoids. Your constipation should be diagnosed as soon as possible. Dehydration, lack of fiber in your diet, pregnancy, inactivity, and medications (such as opioids, iron supplements, or antidepressants) are some factors to consider. It is possible to relieve constipation with laxatives and to prevent it from returning with lifestyle changes.
Crohn's disease - Chronic bowel disease, Crohn's disease causes inflammatory patches in the GI tract anywhere from the mouth to anus, although it is most commonly found on the junction where the small intestine meets the large intestine. According to experts, the exact cause of the disease is unknown; however, it is more common in "Westernized" countries, runs in families, and can be aggravated by diet and stress. There are several symptoms associated with this condition, including diarrhea lasting several weeks, abdominal pain, and weight loss. Around 50% of those with Crohn's disease, notice blood in their stools or mucus in their stools, and some may feel as if they are not able to evacuate completely. Among the various kinds of drugs available for treating arthritis are aminosalicylates, steroids, immunomodulators, and biologics. In addition, surgery is an option.
Diarrhea - Diarrhoea is marked by frequent urgency to go to the toilet as well as loose, watery stools (feces). Sometimes nausea or vomiting can also occur, as well as abdominal pain or cramps. Noroviruses, which are a common cause of diarrhea outbreaks on cruise ships, are a common cause of diarrhea caused by viruses. Salmonella, campylobacter, or Escherichia coli are common causes, as are giardia; various medical conditions (including celiac disease); food intolerances, and certain medications. Loperamide and diphenoxylate slow down bowel movements, while electrolyte solutions treat dehydration associated with diarrhea, which typically occurs after excessive diarrhea. There may also be a need for other medicines, such as antibiotics.
Gastroesophageal reflux disease - Heartburn and acid reflux are also known as GERD. The lower esophageal sphincter, which normally closes tightly to prevent food from flowing back up the esophagus, becomes weakened and remains partially open. This allows partially digested food and stomach acid to leak back up and cause irritation. Regurgitation, heartburn, chest pain, and nausea are the primary symptoms associated with GERD. Antacids, H2 blockers, and proton pump inhibitors are most commonly used to treat GERD.
Get subject wise printable pdf notesView Here



No comments:
Post a Comment
Please don't spam. Comments having links would not be published.